Updates & Changes
Changes in Edition 7.4.0 [April, 2019]
Corrected a few typo's
[p14] High flow oxygen 15 l/min can abort some types of migraine
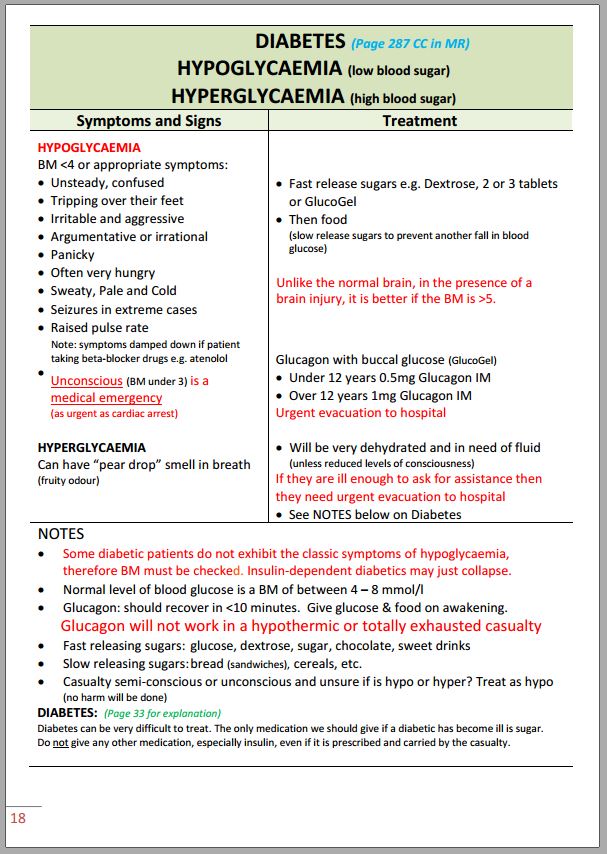
[p18] Updated guidance on managing hypoglycaemia. Also replaced the term 'blood sugar' with 'blood glucose' throughout the text as it is the term now preferred by diabetics.
[p32] Added section on the management of drug overdose and poisoning
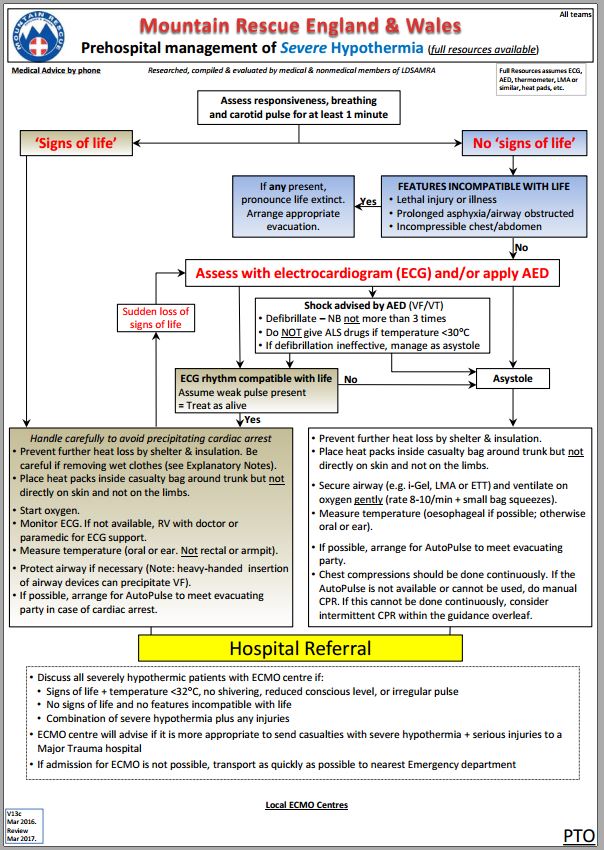
Latest version of hypothermia protocols (now includes Full Resources and Limited Resources)
Changes in Edition 7.5.0 [November 2019]
New cover page
Corrected a few more typo’s
[p7] Following discussions at the November MREW Medical Subcommittee, slightly revised guidance on Primary Survey - Breathing, to clarify the usage of the acronyms TWELVE and FLAPS. TWELVE is in current use by the Ambulance Service and is mentioned in JRCALC. FLAPS has been used by some prehospital organisations. Rather than suggest that this is the absolute standard for MR, changed the title to "THOROUGH ASSESSMENT OF THE CHEST FOR LIFE-THREATENING INJURY. Examine from the Adam's Apple (larynx) to bottom of rib cage for abnormalities (can use acronyms TWELVE and FLAPS as aide memoire)". This releases people who find the acronyms difficult to remember to feel they have to commit them to memory. Also reduced some of the duplication inherent in these two similar acronyms (FLAPS can be incorporated into TWELVE at 'W').
[p50] Updated version of LAMRT Drugs Crib
[p54] Following discussions at the November MREW MSC, replaced LAMRT Diagnosis of Death protocol, with UKSAR ROLE protocol. Although this was derived from the LAMRT version, and is almost identical to it, the new version it has now been accepted by UKSAR, UK Coroners and others, which means that the coroners will be expecting that specific protocol and checklist to have been followed.
Changes in Edition 8.0.n [February 2023]
New version number as completely updated. Page numbering has been revised due to conversion from graphic format and additional text (clearer explanations and new sections). Clinical problems now grouped into Medical and Trauma and more logical ordering e.g. asthma and anaphylaxis are now in consecutive sections. All CPR sections together.
The page numbers listed here refer to the updated version (8.0), not the previous version (v7.6). References have been cited in a few sections in case anyone wishes to read the supporting evidence or is unsure about some of the recommendations.
This document only lists the main changes from the previous version of the book. Small changes in layout or slight rewording without changing the meaning have not been listed here. Everything else is unchanged.
Finally, for an in-depth review of all the medical problems we could come across, see Brugger H, Zafren K, Festi L, et al. Mountain Emergency Medicine. EDRA. 2021.
Page 2 (QR code)
Page 3 (Disclaimer)
Page 7 (Preamble)
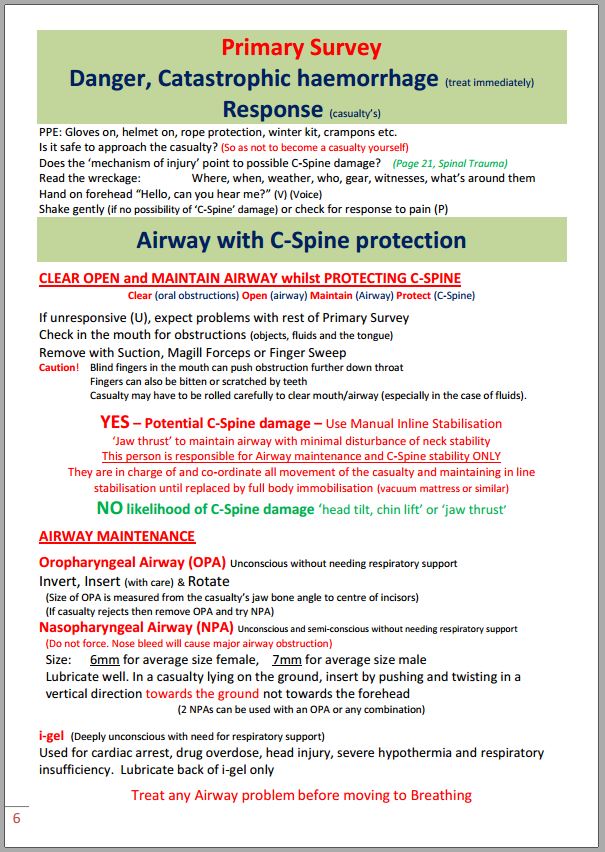
Page 8 (Primary Survey overview)
Page 9 (Primary Survey, Catastrophic haemorrhage)
Page 10 (Primary Survey, Airway with C-spine protection)
Modified initial instruction about C-spine on Mike Greene’s advice. Now states: If casualty is fully conscious and co-operative, tell them to “please keep their head and neck still”. Mike points out that there is no need to place hands on the head and neck if the patient is awake and co-operative until they need to be packaged. This frees up carers for other essential tasks.
Page 11 (Primary Survey, Breathing)
Simplified the examination of the chest for serious injury. In particular, we have now stopped using TWELVE and FLAPS. The observation of many doctors in MR when examining Casualty Care is that it is not well understood by Cas Carers, it forces people to collect some clinical signs that are difficult both to find and interpret e.g neck vein distension, and that some of the features are rare in MR practice (e.g. laryngeal trauma). In addition, reviews about pneumothorax regarding the clinical 2 signs of tracheal shift, sub-cutaneous emphysema and increasing distension of neck veins show that these signs may not be present.
Page 12 (Primary Survey – Circulation)
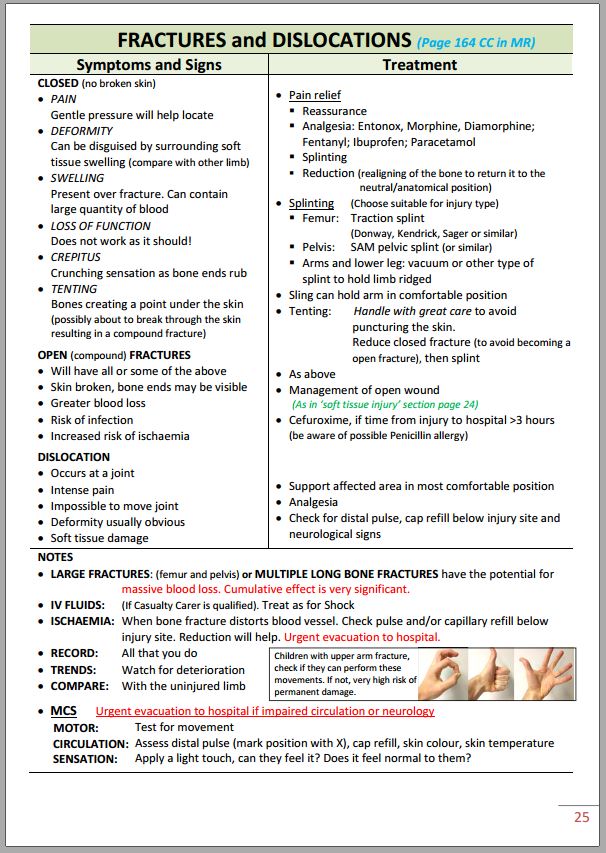
For clarification, changed wording in long bone fractures to: “Do not apply femoral traction splint if hip/knee dislocation, or any ankle injury. If pelvic + femoral fractures, use Pelvic Sling plus Kendrick traction splint for femur (+ see below)”.
Also reworded the additional guidance at the bottom of the page to: “If pelvic and femoral fractures are both present, the pelvic fracture is potentially more serious and takes precedence. Apply a pelvic sling and consider using a traction splint that does not exert pressure against the pelvis in the mid-line (crotch). In MR, this means the Kendrick Traction Device can be used, but not splints that press against the pelvis e.g. Sager”.
For fractures of the pelvis, now refer to “Pelvic Binder”. Previously, the wording was “SAM Pelvic Sling or similar”, which apparently has confused some people who don’t use the SAM but a different device e.g. the Prometheus Pelvic Binder. Reason why fractured neck of femur (FNOF) is not mentioned as an exclusion to using a traction splint: although traction splints e.g. Kendrick are primarily intended for use on a fractured shaft of femur, expert advice from two orthopaedic surgeons is that it can be difficult to tell the difference between a shaft fracture and a FNOF. In addition, as the splint won’t do any harm to a FNOF and will improve comfort, it isn’t a mistake to use them on a casualty with FNOF.
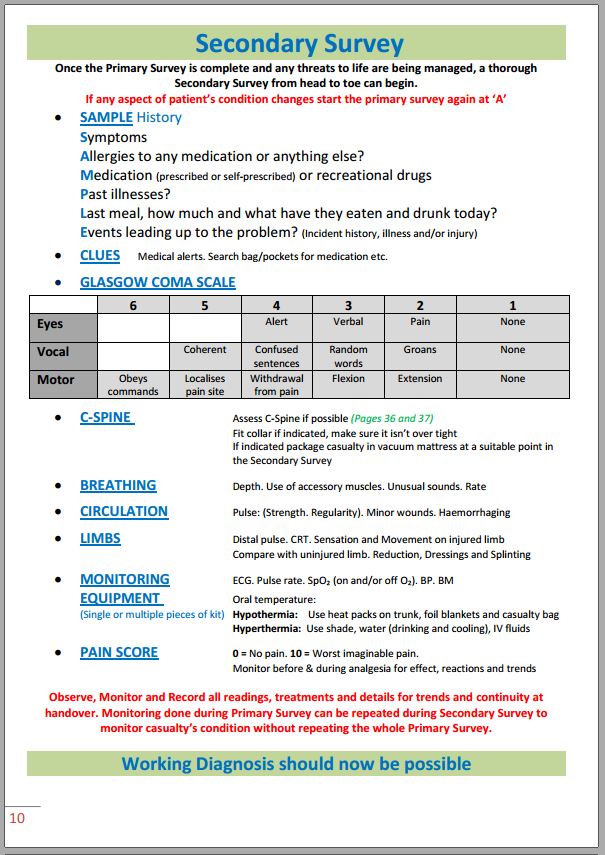
Page 13 (Primary Survey - Disability)
Addition of “C” to AVPU to give ACVPU, where the ‘C’ indicates new onset confusion. Although confusion was recognised as an issue (see below for previous wording), there was no way of highlighting it if just using AVPU. “C” has been added as it is now a component of the National Early Warning Score (version 2) so is increasingly used by healthcare professionals.
Previous wording:
(GCS can be done at this stage if personnel are familiar with it. However, it takes longer and is more difficult than AVPU for a non-medical person so reasonable to leave GCS until secondary survey). NOTE: new onset aggression does not feature in AVPU or GCS but is very significant and should be recorded.
New wording
GCS can be done at this stage if personnel are familiar with it. However, it takes longer and is more difficult than AVPU for a non-medical person, so it is reasonable to leave GCS until secondary survey.
Page 14 (On completion of the Primary Survey)
Added warning that: Unless a problem can be treated completely on the hill e.g. hypoglycaemia, any ongoing Primary Survey problem is an indication for rapid evacuation because, by definition, it is a threat to life.
Page 15 (Secondary survey)
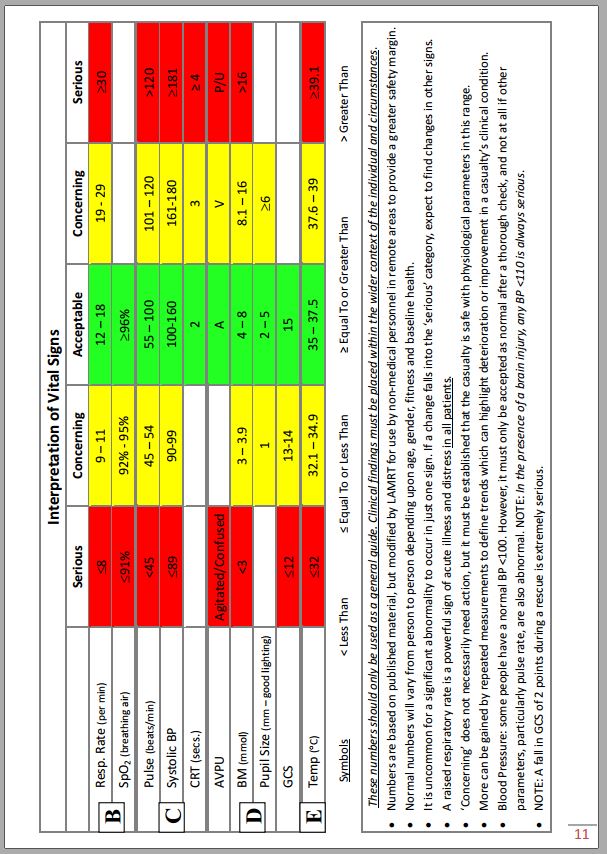
Page 16-17 (Vital signs table)
It is important to remember that this table will be used mainly by non-healthcare professionals in remote locations, where expert help may not be readily available. Therefore, we have maintained the principle that values should be kept more conservative than would be used by healthcare professionals in hospital or in the ambulance service, to provide earlier warning of impending trouble. This will give a bigger time buffer before the casualty becomes extremely ill, will mean teams will call for expert help sooner, and will provide more time for that help to arrive.
There is now very good evidence that a change in respiratory rate is a reliable early warning sign of potential trouble. Therefore, revised the “acceptable”, “concerning” and “serious” values for respiratory rate to bring them in line with national guidance.
BP will still be ranked as serious if above 180 (national cut-off for hospitals and ambulance staff ≥220). We don’t want rescuers to be delaying calling for help until the BP is well over 200, because with the inevitable delay before obtaining expert help, the risk of a serious cardiovascular event when the BP is that high is unacceptable.
Page 18 (Shock)
Reason: “Hypovolaemic” is not wrong, but it’s a medical term that some people may find confusing.
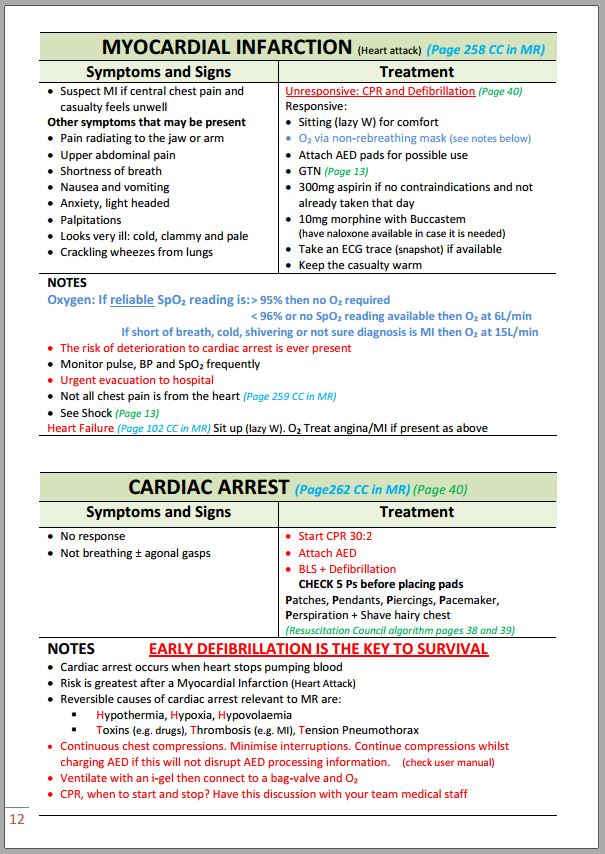
Page 21 (Angina)
Reason: emphasises the urgency (could progress to full myocardial infarction), and that these casualties should not indulge in further exercise.
Page 21 (Myocardial infarction)
Oxygen: If reliable SpO₂ reading is: ≥94% then no O₂ required< 94% or no SpO₂ reading, short of breath, cold, shivering or not sure diagnosis is MI, then O₂ at 15L/min i.e. no extra oxygen or 15L/min
Reasons:
Page 22 (Stroke; Migraine)
Stroke
Migraine
Page 23 (Asthma)
Deleted the phrase saying “or favourable response to medication as shown by a reliable SpO2 reading”. The only possible reason for reducing oxygen flow to a face mask is if there it is in short supply, since it is probably better for the patient to breathe a little extra oxygen all the time, than to breathe a lot for e.g. 20 minutes, until the cylinder is empty, and then just breathe air. Clearly, if enough oxygen is available, then 15 L/min is best in an asthmatic. If it is necessary to reduce the flow, calculation has shown it will probably be safe to go down to 10L /min. Resume 15L/min when possible.
Page 24 (Anaphylaxis)
Slight rewording to clarify the symptoms and signs (e.g. see Resuscitation Council UK. Emergency treatment of anaphylaxis. Guidelines for healthcare providers. May 2021). Grouped the symptoms and signs as A, B, C to make it easier to remember.
Now state, “Do NOT stand the casualty up (can cause cardiac arrest)”. Added “If they tolerate lying flat, raising the legs helps keep the blood pressure up”. There is strong evidence that allowing the patient to be in a position that encourages blood to pool in the legs will allow the blood pressure to drop even further and this can result in immediate cardiac arrest.
Page 25-26 (Seizures and ‘funny turns’)
Slight rewording of last section on heat stroke, fever, infections, drugs & alcohol, stroke to clarify treatment. No new facts added.
Page 27 (Diabetes)
Fast release carbohydrate for hypoglycaemia
Changed Glucogel (25g per tube) to Glucogel (10g per tube). The Glucogel tubes contain 25g of gel but only 10g of that are carbohydrate. Thanks to Nigel Hackney of Glossop MRT for spotting the error.
Page 28 (Hypothermia)
Reason: body oxygen requirements increase if the muscles are working hard by shivering.
Page 29 (Cold-induced soft-tissue injury) – New section.
Page 30 (Heat illness)
Reason: hypoglycaemia could contribute to altered mental state, particularly in someone who has been exerting heavily.
Page 31 (Pregnancy) – New section.
Page 32 (Abdominal pain) – New section.
Page 34-5 (Managing despondent, suicidal, and violent people) – New section.
Page 35-6 (Capacity and consent in MR) – New section.
A basic understanding of this is important for all casualty management, and particularly when caring for people who may not be able to consent to treatment e.g. Drug Overdose and Poisoning, and Despondent, suicidal and violent people.
Page 40-41 (Chest injury)
Removed details of needle chest decompression. It had been included in case there was a dire emergency, but the technique is not perfect, and it shouldn’t be attempted without some training. It certainly is not a casualty care skill.
Added introductory paragraph.
Chest injury is commonly associated with impaired breathing and hypoxia due to damage to the lung(s) and/or chest wall, and the pain of breathing e.g. due to fractured ribs. Massive internal bleeding may also occur.
Added a short paragraph clarifying what pneumothorax is, as it is clear that some MR personnel are unclear exactly what the term means.
Tension pneumothorax
Shortened the list of signs to those that are commonest.
Removed “unequal chest movement”, “±Reduced sound on affected side”, and “distended neck veins”.
Reason: these are difficult signs to pick up, particularly for Cas Carers, and they occur in <25% cases.
Flail chest
Reason: current literature defines flail as three or more adjacent ribs. Looking back through earlier papers, most state three or more adjacent ribs. It may that that multiple fractures in just two adjacent ribs isn’t sufficient to cause significant respiratory embarrassment.
Open pneumothorax
Deleted reference to three-sided dressing being no longer recommended as this should now be well gone from discussions about this topic.
Updated the guidance on dressings to use on these cases, monitoring for the development of a tension pneumothorax, and what to do if it occurs. This is basically to remove the dressing.
Following advice from national experts, added: “In the rare case where breathing does not improve and the casualty continues to deteriorate, carefully push the tip of the little finger of a gloved hand into the hole, up to a depth of about 5cm to release trapped air. Get medical advice, if possible, before doing this”. Although this sounds daunting, there have been cases where the hole in the chest wall has been blocked by blood clot or tissue debris. Inserting a little finger for a limited distance can unblock the hole and release the pressure that has been built up. Note: this is a special life-threatening situation. It is not carte blanche for people to start sticking their fingers into everything!
Page 42 (Head / Brain injury)
New onset aggression after head injury does not feature in AVPU or GCS but is significant and should be recorded on the Cas card.
New wording
New-onset confusion is very significant. Indicate using modified AVPU (ACVPU), where ‘C’ = new confusion (Williams B. The National Early Warning Score and the acutely confused patient. Roy Coll Physicians 2019)
Added key steps in helmet removal.
Page 43 (spinal trauma)
Emphasises that special packaging is required for these casualties including vac mat and lift-and-slide.
Thoracic and lumbar spinal injury – indications for immobilisation. Changed “Presence of painful injuries” to “Presence of painful distracting injuries”. Reason: the spine itself may be painful. However, a particular danger is if other painful injuries are present as these may distract the casualty from being able to report accurately about the spine.
Removed priapism as one of the clinical signs. A recent review (2021) indicates that it is extremely rare.
Removed reference to cervical nerves 3,4,5 control the diaphragm (345 to stay alive). It’s correct, but it’s not possible to count the vertebrae without an x-ray and it’s one less piece of information to have to remember. In practice after a spinal injury, casualties will either be able to breathe, or they won’t.
Page 45 (soft tissue injury and wounds)
Following advice in a recent article in the British Medical Journal (Colmers-Gray IN, et al. Minor injuries: laceration repairs. Brit Med J 2023)
Slight change to immediate care guidance for bleeding wound
Added recommendation to check blood supply, sensation and movement distal to the injury
Added recommendation to consider if any precipitating factors that led to the injury e.g. fainting
Page 47 (Fractures and dislocations – Lower limb)
Changed “Only use Kendrick if concomitant pelvic fracture” to “If concomitant pelvic fracture, only the Kendrick is suitable as it does not push on the pelvis.” Rationale: Explains why this advice is given. Deleted guidance not to use a traction splint in fractured neck of femur. Reason: Although traction splints e.g. Kendrick are primarily intended for use on a fractured shaft of femur, the latest advice from two orthopaedic surgeons is that it can be difficult to tell the difference between a shaft fracture and a FNOF. In addition, as the splint won’t do any harm to a FNOF and will improve comfort, it isn’t a mistake to use them on a casualty with FNOF.
Patella dislocation: added “If in doubt, splint the leg in a comfortable position and leave knee alone for treatment in hospital.”
Reason: in case there is either doubt that it is a simple dislocation, or the Cas Carers on scene haven’t been trained or are unhappy to proceed with repositioning the patella.
Page 48 (Fractures and dislocations – Upper limb)
Changed “Humeral fracture is very painful” to “Humeral fracture may be very painful”. Rationale: Stating categorically that humeral fractures are very painful creates an opportunity for a misdiagnosis if the casualty has such a fracture but is not in a lot of pain. Someone might think that because there is not a lot of pain, it can’t be a humerus and therefore not check for other things e.g. circulation and nerve damage.
Page 49 (facial trauma) – New section
This is uncommon, but LAMRT had a difficult case in late 2022. If it occurs, it can be tricky to manage, particularly the airway. We therefore felt it appropriate to include a section on this.
Page 50 (eye injuries)
Suggestion for an improvised eye shield is helicopter goggles.
Explained the value of antiemetics in eyeball rupture.
Added advice from ophthalmic surgeons that it is safest for all eye injuries to be seen in hospital as soon as possible. The possible exception is if unless the eye returns to complete normality. In this situation, teams should get medical advice.
Page 51 (Drowning)
There is very limited good research evidence to inform clinical practice guidelines for drowning. Therefore, most guidance is based on expert opinion (Bierens J, et al. Resuscitation 2021;162:205-17).
Rescue Issues
Undertake a dynamic risk assessment considering feasibility, chances of survival and risks to the rescuer. Survival after cardiac arrest from drowning is rare and most survivors sustain severe neurological injury (European Resuscitation Council, 2021).
Submersion duration is the strongest predictor of outcome. Outcome worsens with duration >5min (Olasveengen T, et al. Circulation. 2020;142(suppl 1):S41–S91)
Water temp >6°C & submersion >30 minutes: survival/resuscitation is very unlikely.
Water temp <6°C & submersion >90 minutes: survival/resuscitation is very unlikely.
Medical Issues
For drowning to occur at least the face and airway must be immersed.
Froth from the mouth and nose is a bad sign.
Priority is to relieve hypoxia therefore:
CPR for drowning starts with 5 rescue breaths. These can be started in the water.
Page 52 (Bites & stings)
Bites & stings:
Changed “Do not attempt to close wound” to “Do not examine or attempt to close wound”.
Changed “If skin broken, antibiotics may be needed” to “If skin broken, give antibiotics” (this is the latest National Institute of Clinical Excellence guidance)
Added: “Human bites may be more dangerous than animal bites because some microbes in human mouths can cause hardto-treat infections e.g. HIV, hepatitis”.
Changed: “Be alert for anaphylaxis” to “Be alert for anaphylaxis after stings and animal bites”.
Rationale: in several reviews of human bites, anaphylaxis is not mentioned as a potential problem.
Snake bite
Page 54 (Lightning Strike)
Page 62-5 (The casualty with a possible C-Spine injury)
Guidance largely unchanged but laid out slightly differently to make it more readable.
Additional guidance to emphasise the current approach.
Rewording to clarify several areas, particularly on how to apply NEXUS.
Flow chart updated to include the change from AVPU to ACVPU
Added guidance based on recent publications on what to do if the head is not in neutral alignment but leaning to one side. This is because forcing the head to conform to what we normally see can be dangerous.
Added that for unconscious patients with an airway concern or significant facial fracture, it is reasonable to turn the casualty into the lateral position even without knowledge of the C-spine status.
Page 66 (Cardiac arrest overview)
Pages 67 (CPR steps)
Page 68-69 (Resuscitation Council UK algorithms)
Page 70 (Triage Sieve)
This year, all UK emergency services will be moving to a new Triage Sieve. It’s quick to use and does not require people to count pulse and breathing rates. After discussion with the MREW Medical Director, MR teams will use this.
Page 71 (MREW Hypothermia protocol)
Page 72-75 (UKSAR Termination of Resuscitation and ROLE Protocols)
Page 77 (2023 ICAR Avalanche protocol – Update)
Page 78 (MREW Wellbeing information - New)